- Materials in dentistry
- Therapeutic materials
- Surgical materials
- Orthopedic materials
- Types of materials for restorations
- Metals
- Alloys
- Noble metals
- Base metals
The use of innovative materials and equipment in prosthetics has allowed this dental service to reach a new level.
In order for a specialist to provide high-quality treatment, there is a huge selection of materials and tools on the market aimed at improving patient comfort. High-quality materials for prosthetics and dental treatment play a huge role. At the same time, one should not forget about the professionalism of the specialist himself who will carry out this procedure. This reduces the risk of pain and ensures that the manipulations performed will bring the desired effect, and your teeth will be healthy for a long time.
Modern means in dentistry can reduce the likelihood of relapses and inflammatory processes after treatment. In our country today, the level of services is approaching world leaders.
All this became possible thanks to the use of the latest drugs and tools that allow us to provide medical care.
Symptoms and causes of dental hypersensitivity
With this pathology, patients experience increased sensitivity to temperature changes, mechanical and chemical effects.
Painful sensations, as a rule, appear sharply at the moment of interaction with the irritant. Moreover, they quickly pass after its elimination. People with hyperesthesia experience pain when brushing their teeth or eating sweet, salty, hot or cold foods. According to statistics, middle-aged people - 30-50 years old - are most susceptible to pathology. The causes of increased tooth sensitivity are varied and individual. They can be either congenital or acquired. In the first situation, the hereditary factor plays a decisive role, and in the second, the disease appears against the background of prolonged exposure to external irritants (for example, thermal, chemical or mechanical) on the teeth. Among the most common reasons are:
- poorly performed filling or whitening procedure;
- the presence of carious and non-carious lesions of enamel and gum diseases. In this case, the cause of increased sensitivity is due to the loss of layers of enamel and dentin;
- improper (or insufficient) oral hygiene. Some people do not follow the correct technique for cleaning molars and premolars, abuse whitening toothpastes, and use toothbrushes that are too hard;
- exposure of tooth roots as a result of decreased gum level;
- lack of professional cleaning to remove hard and soft plaque from the enamel surface, which contains pathogenic microflora;
- poor nutrition. Excessive consumption of carbonated drinks and other products containing sugar and acids, which have an aggressive effect on enamel and dentin;
- disturbance of phosphorus-calcium metabolism in the body;
- deviations from the endocrine system;
- severe pathologies of the gastrointestinal tract, accompanied by frequent heartburn.
Plastic Safety Standards
For all types of prosthetics, special composite compounds are used, approved after many years of testing. The use of polymers is regulated by GOST 31574-2012. Its requirements correspond to international ones - ISO 4049:1988 for filling materials and ISO 10477:1992 selection of materials for bridges or crowns. The determining indicators of the reliability of orthopedic compositions are the following:
- strength;
- hardness;
- elasticity:
- viscosity;
- plastic;
- fluidity.
Mechanism of action of desensitisers
Desensitizers are recognized as effective drugs for the treatment of hypersensitivity of hard dental tissues. They can affect teeth in different ways:
- mechanical blockade of dentinal tubules. These methods are used by products produced in the form of varnish. When applied, the varnish covers the surface of the tubules with a thin but durable film. As a result, the likelihood of pain is significantly reduced;
- moistening the dentin immediately before placing the filling agent. The drug recreates the moisture content of dentin, which is lost due to excessive drying. As a result, the adhesion of the adhesive is significantly improved as it penetrates deeply into the tubules, guaranteeing the strongest possible bonding;
- precipitation of proteins in nerve endings. The product coagulates proteins. This process makes it difficult for the nerve impulse to pass through, causing the dentinal tubule to close;
- depolarization of nerve fibers. In this case, the dentinal tubules do not close. Due to the disruption of the polarization process, the impulse does not pass and pain does not appear.
Most modern materials are based on a combination of several mechanisms. Some drugs act by only one mechanism, in which case their effectiveness will be significantly lower.
Surgical materials
Suture material is considered one of the most popular in modern dental surgery.
Moscow companies present a huge number of all types of these products. Currently, these types of materials are divided depending on their resorbable properties. There are also differences in the size, shape and strength of needles and threads.
Popular is the copolymer monofilament monoquick, which is a violet thread that has a short resorption period. A week after implantation, it maintains strength indicators within 50%. After 2 weeks, this figure drops to 20 percent. Can be used as a synthetic analogue of catgut.
Types of Desensitizers
According to their composition, there are four main types:
- unfilled with HEMA content. The active ingredient is hydroxyethyl methacrylate. It acts as a dentin wetting agent and reduces the collapse of collagen fibers. As a result, the adhesive penetrates better into the dentin tubules. In addition to hydroxyethyl methacrylate, the composition includes water and fluorine. As an antiseptic, a solution of chlorhexidine is often added, which has a bactericidal effect. Apply the product using microbrushes, using gentle rubbing movements. Excess material is removed by a tow truck;
- filled with HEMA content. A distinctive feature of this group is the presence of fillers whose particle diameter is less than 7 nm. The active component is a compomer or ormoker (filler). In addition, the composition contains antiseptic substances and fluoride ions, which reduces the rate of formation of soft plaque. Apply the product using microbrushes, then blow with a stream of air. Upon completion, they are illuminated with a photopolymerization lamp;
- containing weak acids and surfactants. The surfactants included in the composition wet the dentin before applying the adhesive. Benzalkonium chloride acts as an antiseptic. Due to a weak acid, the dentin surface is cleaned;
- acting to form complex salts on the surface of dentin. Preparations of this group form macrocrystals of complex salts on the surface of the tooth, which as a result turn into an indelible film. The essence of the desensitizing effect is the mechanical blocking of the dentinal tubules to prevent further movement of fluid through them. The preparations are easy to use: they are applied to a previously cleaned tooth using microbrushes, distributing them using a stream of air.
Dental composite materials (composites)
Dental composites today are the main class of restorative (filling) material. The advantages of composites over many other filling materials are their high strength, which allows them to be used in any clinical situations (both on anterior and chewing teeth); high and flexible aesthetic characteristics that allow you to manipulate the color of restorations and their gloss over a wide range of values; high technology when performing restorations; minimal polymerization shrinkage.
However, composites, even with the maximum content of inorganic filler, still have some shrinkage during curing, a fairly high coefficient of thermal expansion and less rigidity than that of dental tissues. These disadvantages of composites contribute to the appearance of marginal gaps between the filling and the dental surface, leakage of oral fluids through these gaps and, as a result, depressurization of the cavity. This leads either to the loss of the filling (damage to the restoration) or to the development of secondary caries. The disadvantages of composites are eliminated by the use of adhesives (adhesive systems ensure “gluing” of the composite to dental tissue) or other techniques. Therefore, polymerization shrinkage of dental composites is currently not a problem in restorative dentistry.
By definition, a composite material is a mixture of several dissimilar components. In the case of dental composites, it is a mixture of filler (usually inorganic) and an organic matrix, and the filler content is very significant (at least 30% by volume; with a lower filler content, the material is usually classified as a “low-filled polymer”).
Additional components of the organic matrix (in the initial state) are a polymer inhibitor (to increase the curing time and shelf life of the material), a catalyst (in the case of chemically cured composites; a separate component in the form of a paste or liquid), a photoinitiator (in the case of light-cured composites), an accelerator polymerization (in chemically cured composites), ultraviolet light absorber (to improve light stability) and dyes.
Typical fillers for dental composites are amorphous silica, quartz, barium glass, strontium glass, zirconium silicate, titanium silicate, oxides and salts of other heavy metals, and polymer particles. Modern technologies for the production and introduction of fillers include: improved grinding technologies to produce smaller particles; technologies for producing chemically deposited filler particles (the so-called sol-gel process; allows you to obtain filler hybrids); strengthening of composites with fibers (reinforcement; but this leads to a decrease in the transparency of the composite); introduction of porous (chemically deposited) fillers and three-dimensional structures (to reduce shrinkage stress); introduction of fillers with anti-caries properties (primarily those that release fluoride; however, the limitation is the low permeability of the organic matrix of the composite); technologies for modifying the surface of filler particles to allow copolymerization with an organic matrix (for example, alkoxysilanes); nanotechnology.
The size and amount of filler are the basis of the most common classification of dental composites. Based on the size of filler particles, composites are distinguished: macrofilled, macrophiles (10-100 microns); midin-filled (1-10 microns); mini-filled (0.1-1 microns) micro-filled, microphiles (0.01-0.1 microns); hybrid (contain macro- and microparticles); heterogeneous (conventional or hybrid composites with additives of particles of polymer material 1-20 microns in size).
Based on the content of filler particles (the degree of filling of the dental composite), highly filled composites (more than 60% by volume), medium-filled composites (40-60% by volume) and lightly filled composites (30-40% by volume) are distinguished. The polishability, abrasion resistance and color stability of the dental composite depend on the size of the filler particles. Strength, degree of thermal expansion and polymerization shrinkage depend on the degree of filling.
Recently, so-called nanocomposites have been identified among dental composites, which can be conditionally considered as hybrid microphilic (microhybrid) materials. In nanocomposites, “nanosized” particles (nanomers), which have a size of up to 0.1 μm (100 nm), are used as fillers. Nanomers tend to aggregate to form nanoclusters, so in reality a nanocomposite contains a mixture of nanomers and nanoclusters as a filler. Nanoclusters behave like individual particles, and modern technologies make it possible to control their size and shape. As a result of combining nanometers and nanoclusters in one material, the material has a high fullness (more than 75%), which ensures high strength. In conventional hybrid dental composites, during the process of abrasion, strong filler particles leave the surface and leave behind “craters,” which reduces the shine of the restoration or filling. In the case of abrasion of nanocomposites, nanoclusters are removed not entirely, but their smaller components, which allows the nanocomposite to have a more durable shine and good polishability. Nanocomposites of the latest generations (for example, Estet-X) contain three filler phases: nanoparticles, midiparticles phase and miniparticles phase. The ratio of the three phases is strictly dosed. The name “micromatrix” has been proposed for such nanocomposites.
The basis of the organic matrix of dental composites (before the stage of their curing) are monomers, the molecules of which contain fragments of epoxy resin and two methacrylate groups. It is known that methacrylic acid and its derivatives easily enter into polymerization reactions (for example, with the formation of polymethyl methacrylate, which is usually called “plexiglass”), and the reaction proceeds by a free radical mechanism. The first monomer of this type was patented back in 1959 (GMA monomer) and since then GMA and its derivatives have been included in almost all modern dental composites and adhesives. The reason for the dominance of monomers of this type is the relatively low polymerization shrinkage (about 6% in pure form), rapid curing, low volatility, and good mechanical characteristics of the final polymer.
Polymerization initiators are substances that generate free radicals when exposed to light or chemically. Therefore, according to the polymerization (curing) method, dental composites are divided into light-curing composites (light-composites, photo-composites, gel-composites) and chemical-curing composites (self-curing).
Chemically cured dental composites are either paste-paste or powder-liquid systems. The reaction that initiates polymerization (curing) is the interaction (after mixing the starting components) of the amine and benzoyl peroxide with the formation of free radicals. The rate of polymerization depends on the number of initiators, temperature and the presence of inhibitors. The main advantage of such dental composites is uniform curing, regardless of cavity depth and filling size.
Light-curing dental composites are a one-component initial form (paste or flowable material). A light-absorbing substance (photoinitiator; the most traditional is camphoroquinine, maximum absorption spectrum is 475 nm), which, when absorbing light with a wavelength of 400-500 nm (blue light), forms free radicals, is used as an initiator of polymerization (curing). Light composites do not require mixing (therefore they are more homogeneous), they allow modeling of the restoration (filling) before light curing, and the absence of chemically active additives (the absence of amines) gives them color stability and aesthetics. However, it should be taken into account that the degree and depth of polymerization may be non-uniform and depends, first of all, on the transparency and color of the composite, and the power of the light source. Typically, layer-by-layer application and curing of the dental composite is carried out, which makes it possible to reduce shrinkage and stress in the matrix and more accurately select the color of the restoration (filling).
The light source for curing dental composites is usually conventional halogen lamps (halogen photopolymerizers). Their disadvantages are the small “useful” component of radiation (less than 2%), the need to use an interference filter that cuts off stray thermal radiation, and a fan (to remove heat). Recently, emitting LEDs are increasingly used as light sources, the emission spectrum of which practically coincides with the absorption spectrum of camphoroquinone, and which do not have all the disadvantages of halogen lamps.
A separate group of dental composites with which teeth are filled are restoration (filling) materials of a “hybrid” type – compomers.
Compomers are light-curing restoration (filling) materials that combine the main advantages of composites (ease of use, strength, aesthetic properties) and glass ionomer cements (chemical adhesion to tooth tissue, good biocompatibility, fluoride release). The term “compomer” comes from a combination of the words COMPOSITE and glass ionomer. The initial (before polymerization) organic matrix of compomers is a monomer (acid methacrylate), the molecule of which contains methacrylate (like a composite) and acid (like glass ionomer cement) groups. Compomer fillers are fluoroalumosilicate glass particles. Acid methacrylates can simultaneously cure by the free radical mechanism (as in the case of polymerization of light-curing composites) and by the ion exchange mechanism (as in the case of glass ionomer cements). Curing of compomers occurs only due to light-induced polymerization. Curing similar to glass ionomer cements (requiring the presence of water to dissociate acid groups) occurs only in areas of the material in contact with water.
Compomers differ from classical hybrid glass ionomer cements modified (reinforced) with composites. In the latter, the ion exchange reaction, which initiates the curing of the material, is the dominant part of the entire curing process. In contrast, compomers are materials that contain the main components of glass ionomer cements in quantities insufficient to maintain the ion exchange reaction under normal (anhydrous) conditions. Although compomers were developed to combine the best properties of resin composites and glass ionomer cements, their behavior is more similar to that of dental composites.
Disregarding the basic physical and chemical characteristics of materials, the entire range of modern dental composites, according to the features of their application, can be divided into 5 main groups.
- Universal composites with one-color color restoration concept. This group includes almost all chemically cured composites and some light-cured composites.
Charisma PPF. Chemically cured composite material. Used for filling, restoration of the crown part of the tooth, fixation of mobile teeth.
Ceram X. Light-curing nanocomposite for small restorations (fillings) of chewing teeth. The material has been optimized for highly aesthetic restorations with a minimum number of shades.
- Versatile composites with a two-layer color reproduction concept. Such composites (restorative systems) include one or more dentins, which provide the creation of the internal structure of the tooth, and a set of enamel shades (including a transparent cutting edge), which ensures the refraction of light on the tooth surface. These materials make it possible to achieve fairly high results in the restoration of anterior and chewing teeth, but still somewhat limit the creative possibilities of the dentist in reproducing color.
Filtek Z 250 (Filtek Z 250). Aesthetic light-curing microhybrid composite. Contains an increased amount of smaller particles. It is used for filling cavities of all types in the frontal and chewing teeth, making veneers, restoring the coronal part of the tooth, and splinting. Has 15 different shades.
Spectrum TPH. Light-curing microhybrid composite. The filler (barium glass and sintered silicon) has 2 fractions of 0.04-0.4 microns and 0.8-1 microns with a filling of 55-60% by volume. Due to the successful combination of aesthetic and mechanical properties, they are used for restoration (filling) of all types of defects in hard dental tissues. An entire generation of dentists grew up on this material and mastered the basics of cosmetic restoration techniques.
- Restoration materials with a three-layer color reproduction concept. Restoration (filling) materials of this group are “artistic” systems. The range of shades includes a wide range of opane (opaque) dentin shades, basic tooth body shades and a set of transparent enamels.
Estet-X. Light-curing micromatrix composite material. The filler is presented in the form of three phases (up to 2.5 microns, 0.4-0.8 microns and nanoparticles 0.01-0.02 microns), the ratio of which is strictly dosed. Has extremely high aesthetic capabilities. Used by dentists who focus primarily on achieving high aesthetic results. With the same strength and color stability as, for example, Spectrum TRN, it is washed 3 times less, does not require updating the gloss and has 2 times less shrinkage (which justifies the high cost of this material).
Filtek Supreme. Light-curing nanocomposite material. The filler (zirconium silicate) is presented in the form of nanoparticles (0.02-0.75 microns in size) and nanoclusters. The technology allows you to control the size of nanoclusters (create a given size) and in this way influence the strength, polishability and polymerization shrinkage of the material. A universal restoration (filling) material that combines the mechanical properties of microhybrids and the aesthetics of microfills.
The choice of a dentist in favor of a specific material from these three groups is associated with a combination of several factors (price of the material, cost of work, time spent working with the patient and the qualifications of the doctor, the final aesthetic result). For relatively simple restoration (filling), dental composites of the 1st and 2nd groups are predominantly used. If the dentist is not very limited in time, and his patient is less limited in funds, he can use materials of the 3rd group, which provide him with wider opportunities.
- Dental composite materials for restoration (filling) of chewing teeth. The main requirements are high resistance to abrasion and deformation under chewing load.
Quixfil. A light-curing composite material designed specifically for restoration (filling) of chewing teeth. It has a high (30% greater than most other composites) fullness, due to which it has increased hardness and low polymerization shrinkage. The filler (glass) is presented in the form of two fractions: 1 and 10 microns. A specially developed organic matrix (monomer) provides a large depth of polymerization (the thickness of the polymerized layer is up to 2.5 mm). The high level of transparency of the material makes the restorations (fillings) slightly different from natural enamel, which makes it easy to determine the location of the material in complex restorations of lateral teeth. Has one universal shade.
- Liquid-flowing composite materials. Used for filling small cavities, fissures, and cervical defects using the minimal intervention technique. For small cavities, shrinkage and subsequent marginal permeability are not as important as for large cavities, so flowable materials are optimal for adapting the restorative material to the cavity. All fluid-flowing composites are classified as medium- and lightly filled (filler content less than 47%). Liquid-flowing composites have the property of thixotropy (fluid under the influence of instrument load and viscous after the load is removed), therefore, before polymerization, they do not flow beyond the boundaries of the cavity, even on the teeth of the upper jaw. Another important property of flowable composites is their low modulus of elasticity. This allows them to compensate for the stress that occurs under the influence of chewing load at the “filling-tooth” border (which is especially important when restoring cervical defects).
X-flow. A universal, flowable, light-curing composite. Adapts to cavity walls without the use of hand tools. The filler (38% by volume, particles 1.6 microns in size) is represented by special glass, highly dispersed silicon dioxide, titanium dioxide. Used for filling small cavities of anterior and lateral teeth (without chewing load), sealing fissures, and restoring shallow cervical defects. Can be used for fixation of orthopedic structures (for example, indirect veneers), provided there is light access to the tooth/restoration interface. Has a number of shades.
Filtek Flow. Liquid-flowing light-curing composite. Filler content is 47% by volume, particle diameter is 1.4-1.6 microns. It has high wear resistance and is compatible with other composites. Has a number of shades.
Dyract Seal. Light-curing compomer material (sealant), developed specifically for filling (sealing) fissures. Thanks to its good fluidity and ideal wetting ability, it penetrates deeply into recesses and fissures and ensures a high-quality marginal seal. Abrasion resistant. Being a compomer, it releases active fluoride for a long time, which provides additional protection for dental tissues.
Make an appointment with the best dentists in Moscow!
Popular representatives
Today, the dental market offers many desensitizers from various manufacturers. They act on the basis of one or a combination of several mechanisms, so the effectiveness of the funds varies significantly. The greatest demand is:
- Desensitizer gluma. It is produced by the pharmaceutical company Heraeus Kulzer. Country of origin: Germany. The drug is characterized by an immediate effect and does not require photopolymerization. Gluma desensitizer reduces the sensitivity of dentin by closing the lumen of the dentinal tubules. It contains HEMA, which increases the penetration depth to 200 microns. The achievement of the result is due to the coagulation of dentinal fluid proteins inside the dentinal tubules. The drug is used to treat hyperesthesia of the necks and other areas of the teeth when desensitizing toothpastes are ineffective.
- Shield force desensitizer. It is produced by the pharmaceutical company Tokuyama Dental. Country of origin: Japan. The product provides reliable sealing of dentinal tubules and creates a thin and durable film on the surface, which makes subsequent erosion and abrasion of exposed dentin difficult. It is made on the basis of two reliable monomers, due to which it is characterized by high performance characteristics (tightness and wear resistance). Tokuyama desensitizer guarantees an immediate and lasting desensitizing effect. The drug is often prescribed to patients suffering from dentin hypersensitivity. Due to the instant desensitizing effect, it is possible to use the paste not only for the treatment of dentin hypersensitivity, but also as a preventive measure to prevent the development of postoperative sensitivity.
Application of polymers in dentistry
All plastics for orthopedics can be divided into groups according to the functions they perform.
- Materials from which dentures are made
- Plastic compositions for impressions and forming models for casting, creating trays, protective caps and temporary crowns.
- Clinical agents – sealants, filling compounds and agents for adhesion at the junction of the material with the dental tissue.
There are signs that determine whether polymer can be used in dental prosthetics. The composition should not absorb water while constantly being in a humid environment. In a chemical compound, the residual amount of monomers that have not entered into the polymerization reaction is regulated. During use, they are washed away, having a harmful effect on the body. The dough for pressing should be homogeneous. Temperature and pressure during the process of molding and curing the workpiece affect the quality of artificial teeth and the absence of micropores. All these characteristics are met by special formulations. The basis of orthopedic plastic is a basic polymer. Fillers are substances that give the material special properties:
- Fillers – flour from silicon minerals with high hardness, glass, hydrosilicates.
- Plasticizers – impart elasticity and prevent aging in light.
- Dyes and pigments that create imitation color.
- Initiators and activators designed to continue the polymerization reaction of individual free radicals.
GOST determines that the total amount of fillers should not exceed 50%.
Desensitizer coating in Moscow
Specialists from the Moscow clinic “A-Medic” can apply gluma desensitizer coating. They are highly qualified and have extensive experience in this field, which guarantees a positive result. The cost of the service is significantly lower than in other private clinics in Moscow. You can view the price list on the official website of the A-Medic clinic. To make an appointment with a dentist, just call the numbers provided or leave a request online (indicating your name and contact number).
Requirements for the materials from which the base of the prosthesis is made
All parts of the foreign plate of false jaws, correction of congenital defects require a soft pad that does not cause irritation of the internal membranes. Elastic materials are an integral part of the prosthesis. The synthesis of polymers with specified properties ensures the selection of a basis for removable plate jaws. The finished plate should fit tightly to living tissues without injuring them. When installed in the oral cavity, the prosthesis should change its shape slightly and be elastic. Plastic should not have its own smell, taste, and should be easy to clean from plaque without changing color. The industry produces dental plastics of several types:
- acrylic;
- polyvinyl chloride;
- rubber;
- fluorine rubber.
Dental polymers for the clinic
Before removing a diseased tooth, it is treated for a long time, trying to save it. Filling compounds, corrective onlays, and veneers are used here. It has been experimentally established that copolymer polymers are better suited than other materials for tooth repair at any stage of caries. The seal is subject to harsh operating conditions:
- bears an equal load with natural biomaterial, while being a foreign body.
- The filling is exposed to the surrounding, humid-aggressive environment.
- The destruction of the material occurs under the combined factors, the filling falls out, which indicates low adhesion between the filling material and the bone tissue.
Studies have shown that the initial copolymer methyl methacrylate had weak adhesion and a high coefficient of thermal expansion. The new material included epoxy resins. The resulting putties were devoid of the listed disadvantages, but hardened for a long time. Positive properties were combined by the synthesis of epoxy-methacrylic copolymers. This filling material suited to practitioners is known as Bis-GMA or acrylic oxide. With its advent, it became possible to eliminate chips on the enamel and form a cutter on the pin. The addition of fillers made it possible to obtain a paste-like composition without the release of volatile toxins. Dentists consider nanocomposites to be the best material for dental treatment. One of them is a compomer - a universal composite of monomer, polyacrylic acid and resin, plus amine and benzoyl peroxide. The composition is glass ionomer cement, homogeneous, durable, and is installed on chewing teeth.
Fixed decorative microprostheses
Irregularities and defects of teeth in the smile area can be corrected. Long-term treatment or quick adjustments are possible with the help of special dental plates - veneers. Anyone can flash a white-toothed smile. Each such component is a separate microprosthesis that veneers the tooth.
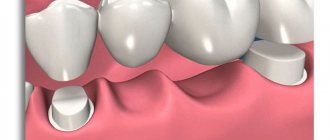
Necessary procedures before bone augmentation
Once a molar or premolar is removed, the bone is no longer subject to regular stress, which over time causes it to atrophy and lose volume. Along with this, inflammatory processes appear in periodontal tissue. As a result, the more days that pass after the loss of a molar or premolar, the more the bone begins to become deficient. Against this background, it becomes much more difficult to carry out implantation.
The technique used to increase bone tissue volume is selected individually in each clinical case. To do this, the dentist first evaluates the oral cavity and, if necessary, prescribes instrumental diagnostics. It often happens that the need to use another technique arises only during the period of surgical intervention. Due to this, the specialist must be aware of all types of osteoplasty and be able to apply them in practice.
Type of osteoplasty
Below are the main types of osteoplasty to understand for which surgical interventions a specific type of material is used:
- autotransplantation. This is a procedure that involves moving a tooth from one place to another in order to fill a visually and functionally significant defect. Eighth molars (wisdom teeth) are most often transplanted. As a result of the operation, the bone tissue becomes significantly wider;
- sinus lift. This is a surgical intervention that is performed on the upper jaw in order to increase the length of bone tissue in case of its deficiency.
It is possible to increase the volume of bone tissue through the use of materials of synthetic origin. Barrier membranes are used to fix transplanted bone tissue or to protect a person’s bone tissue after a molar or premolar has been removed. Allografts are used to restore bone tissue. The most common are autografts.
Types of modern denture plastics
Centuries of experience in the use of rubber in the production of false jaws have revealed many disadvantages of dentures. The material was elastic and porous; it collected food debris in the pores, and their rotting caused a foul odor and irritation of the oral mucosa. There were other important reasons that forced us to look for a new material, more hygienic. In practice, it has been found that plastics based on acrylates most fully meet the task of prosthetics. Thermoplastic material does not contain toxins and does not cause allergies. The polymerization reaction proceeds most completely in them, leaving no single monomers.
Polyamide (nylon)
The structural shape of the polymer is linear, but resembles a flat zigzag. The structure and hydrogen bonds provide a high melting point. ~NH-(CH2) 6-NH-C(O)-(CH2)4-C(O)~ has a main radical, the amide group -NH-C(O)-. Its association with an aromatic or aliphatic ring provides strength, rigidity, resistance to high temperatures and complete neutrality to chemicals. Patented composition name Valplact, available in 4 color options.
Polyoxymethylene (acetal)
A synthetic resin with a linear structure is rolled into molecular balls. The strength of the polymer rivals that of metal. Chemical formula [-CH20-], polyformaldehyde, polymethylene oxide. Solid substance, molecular weight 10,000-30,000 units. The prosthesis is formed by casting. In dentistry, the material is used in its pure form, without chemical additives. The composition is elastic, fits tightly to the teeth, securely fixing the prosthesis. The proprietary product name is Dental D.
Polypropylene "Lipol"
The odorless and tasteless substance has the structural formula [-CH2-CH(CH3)-]. CH3 groups, methyl, are arranged randomly (atactically) or regularly in the chain, an isotactic polymer with a rigid structure. It is used in dentistry under the name “Lipol”. The material is budget-friendly, available in transparent and pink granules. When making a prosthesis, coloring is determined by the proportions of the compositions.
Ethylene vinyl acetate
Flexidy thermoplastic copolymer is synthesized from vinyl acetate and ethylene. Used to make protectors for sports and mouthpieces for diving. The polymer is available in hardness levels of 80.65 and 50 units. In dentistry, a soft transparent composition is used to correct bites. The product care kit includes fragrance liquids.
Polyvinyl chloride materials
Compounding vinyl chloride with another monomer produces a dental polymer. Powder and liquid are used to mold the prosthesis. The powder is a copolymer of vinyl chloride with butacrylate with a titanium dioxide additive. Prepare the dough by adding dioctifthalate. The domestic material, called Eladent-100 or PM-01, is used for the manufacture of gaskets and double dentures.
Silicone
The polymer consists of 3000-10000 silane units and relates to oxygen-containing organosilicon compounds. The material is absolutely non-toxic for humans. A denture made from it does not injure the cavity, fits perfectly and is used only as a base lining for teeth made of hard acrylate. A gasket is prepared from elastomer at the installation site. Removable dentures made of silicone are easy to install, they are indistinguishable from the natural dentition, but require frequent replacement - they wear out. In addition, the load on healthy teeth increases; the material has strong shock-absorbing properties. Silicone polymer materials in dentistry are known under the names Ortosil, Mollosil, Molloplast-B.
Fluororubbers, polyphosphazene fluorelastomers
The elastomer in question does not have the disadvantages of conventional rubber - poor shock absorption and a short service life of the prosthesis. The material reliably connects rigid parts, does not absorb odors and is not subject to rapid wear. The trade name of the composition is Novus, supplied in plates laminated to film, stored in the refrigerator.