Why can odontogenic sinusitis occur?
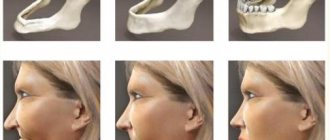
The maxillary (maxillary) sinus is a cavity with bony walls that is located inside the upper jaw. The cavity communicates with the nasal cavity through the anastomosis, which is located on the side wall of the sinus facing the nasal cavity. The lower wall has contact with the upper teeth. Quite often (in about 15% of cases) the apex of the tooth root lies directly under the mucous membrane of the bottom of the maxillary sinus, and there is no bone septum between them.
When an infection enters the maxillary sinus, inflammation of its mucous membrane or sinusitis occurs.
There are two ways of infection:
- rhinogenic - through the nasal cavity. In this case, the infection penetrates from the nasal cavity through natural or artificial (after surgery) communication;
- odontogenic - through the tooth or tissue around it.
Odontogenic sinusitis most often develops slowly against the background of chronic infection in the area of the tooth root. As a result of chronic inflammation, a cyst forms in the root area, which destroys the barrier between the sinus and the tooth. Pathogenic microbes gradually penetrate the sinus mucosa, causing inflammation.
Also, odontogenic sinusitis can occur as a result of the actions of the dentist. Often, after the removal of the upper tooth, the thin barrier between the sinus and the oral cavity may be damaged. As a result, a gateway for dental infection appears. In this case, the anatomical features of the patient with a thin bone septum between the sinus and the tooth root or its complete absence are of key importance.
Infection can occur when cleaning the canals and filling them. In some cases, the filling material gets inside the sinus, causing the formation of fungal sinusitis, and the zinc contained in the filling material promotes the growth of mold fungi (Aspergillus, Mucora). Also, odontogenic sinusitis can develop after the sinus lift procedure and the installation of dental implants in the upper jaw.
Symptoms of perforation of the maxillary sinus floor
If the bottom of the maxillary sinus has been pierced as a result of treatment, the dentist should pay attention to the following symptoms:
- The appearance of air bubbles in the wound, the number of which increases as you exhale.
- Changing the timbre of the voice towards nasality.
- Bloody discharge may appear from the nose.
- The instrument the dentist was using falls into the perforation.
If we are talking about an old injury, then in this case chronic sinusitis develops due to an infection caused by a foreign body in the sinus. The main symptom of such sinusitis is pain in the sinuses and teeth. In addition, swelling appears, which can greatly interfere with nasal breathing. A purulent bloody secretion is discharged from the nose.
What to do if your teeth hurt and it’s hard to breathe with sinusitis? Contact your dentist as soon as possible. A sore tooth can very quickly lead to chronic sinusitis, a headache and a deterioration in overall health.
Complications
With odontogenic sinusitis, a chronic inflammatory process occurs. Dental microflora appears in the sinus, not typical for the upper respiratory tract, which can destroy bone tissue. Due to the fact that the paranasal sinuses have contact with the orbit and brain, odontogenic sinusitis can lead to severe complications:
- intraorbital (orbital phlegmon, ophthalmitis, optic nerve neuritis);
- intracranial (meningitis, encephalitis, brain abscess).
Therefore, at the slightest suspicion of this disease, you should consult a doctor.
Dimensions
The size of the cyst does not affect the severity of symptoms. Large formations may not cause inconvenience. It is much more important where exactly the tumor is located :
- Those located in the lower section of the sinus cause less discomfort.
- But even a small formation located in the upper wall can lead to complications and headaches.
This is due to the close location of the cyst to the branches of the trigeminal nerve.
Recording of a webinar from a doctor of sciences on the topic:
Treatment
The treatment of odontogenic sinusitis requires an integrated approach. As a rule, treatment requires the simultaneous participation of an otolaryngologist and a dentist. Isolated antibacterial and conservative therapy lead only to temporary relief of the condition and removal of the severity of the process.
For a complete recovery, it is necessary to eliminate the source of infection - remove or treat the causative tooth while simultaneously sanitizing the inflamed sinus.
In case of foreign inclusions in the sinus (filling material, sinus lifting material, fungal bodies), their complete removal is necessary. For this, endoscopic techniques are used. They allow you to remove these formations through the nasal cavity. If there is a connection between the sinus and the oral cavity (oroantral fistula), it must be closed using special bioinert collagen-based membranes and mucosal flaps.
Consequences of deletion
For successful recovery after removal of the cyst, the patient is hospitalized. It lasts no more than 2 weeks:
- Every day the nose and sutures are treated and washed with an antiseptic.
- The patient takes antibiotics (broad-spectrum), antihistamines and, if necessary, painkillers.
- The patient will be offered to undergo a course of physical treatment aimed at resolving the swelling.
If the incision heals at a normal pace, the stitches will be removed after 7 days. But in general, rehabilitation will take up to 4 weeks.
During this period, the patient must follow a number of rules :
- Maintain oral and nasal hygiene.
- Rinse your mouth with plain water every time after eating.
- Do not pick your nose or put your fingers in your mouth.
- Reduce physical and thermal stress on the body. Therefore, stop playing sports for a while, do not bathe in hot water, and do not eat hot and spicy foods.
Important! At first, swelling of the lips and cheeks, numbness, and poor sensitivity in this area may persist. It happens that the sense of smell deteriorates for a while, breathing through the nose becomes difficult, and discharge appears. This is a temporary post-operative effect that will go away within a week.
Preventive measures
During the postoperative period, it is better to eat non-solid food at room temperature, so as not to irritate the nervous system and not fully restored tissues.
After and before the course of treatment, it is allowed to use traditional medicine.
Here are a few of them:
- The leaf of any plant must be washed and placed in the refrigerator, keeping it there for at least 3 days. Then the juice is squeezed out of it, mixing the resulting substance with water and instilling 3-5 drops of the resulting mixture into the nostrils several times a day.
- 2 gr. mumiyo and 5 ml. glycerol dissolves in warm water. Place this solution in the nostrils 3-5 times a day.
- Make an infusion of eucalyptus, tea and honey (in equal parts). The nasal passages are instilled in the morning, afternoon and evening.
Their individual use will not give great results, but together with other methods they provide a significant effect, reducing the size of the tumor and clearing the ducts. Plus, they must be agreed upon with the attending physician.
Soft tissue injuries
Damage to soft tissue is a common occurrence in the practice of a dental surgeon. For example, careless or incomplete detachment of the gum when inserting the cheeks of the forceps under the gum and further advancement will lead to stretching of the tissue with subsequent rupture. When forceps are applied to the edges of the alveolus and the gum is captured, crushing and even tearing off the marginal part of the gum occurs. Insufficient detachment of the circular ligament leads to rupture of the gums during removal of the tooth from the socket. Damage to the tongue, tissues of the floor of the mouth, cheeks, and palate occurs when the elevator slips during tooth dislocation.
Prevention of soft tissue damage
Prevention of damage to soft tissues is quite simple and consists, firstly, in careful exfoliation of periodontal tissues and careful handling of instruments in the oral cavity, secondly, in peeling off the gums to a sufficient depth, and thirdly, in using instruments for their intended purpose. When inserting the elevator blade and during tooth dislocation, it is necessary to block the direction of possible sliding of the tool with the finger of your free hand.
Treatment of soft tissue damage
If the soft tissue damage is not accompanied by bleeding, the tooth extraction should be completed, and then the edges of the wound should be brought together with sutures. If there is bleeding, it is necessary to stop it by ligating the vessel in the wound, bringing the edges of the wound together with sutures. In case of a blind wound, sutures are placed on the bottom of the mouth and tongue, after which the wound must be drained for 12-24 hours by inserting a rubber or polyethylene strip into it. When the gum edge is torn off exposing the alveolar process, it is necessary to cover the exposed bone surface. To do this, two vertical incisions are made in the gums to the arch of the vestibule of the mouth, and the mucoperiosteal flap is peeled off. In order to mobilize it, the periosteum is crossed. After this, the mucoperiosteal flap is lowered and fixed with sutures so that it covers the exposed area of the alveolar process. The second option is to form a mucoperiosteal flap in the area of the vault of the oral vestibule and move it to the area of the gum defect.
Tooth root fracture
A tooth root fracture can occur due to: • an error when choosing a tool for tooth extraction; • violation of the rules for the rational use of tools; • features of the anatomical structure of the tooth (long, thin curved roots, root divergence).
Prevention of tooth root fracture
Prevention of root fracture comes down to following the recommendations described above. The first dislocation movement should be made towards the thinner and less durable alveolar wall. Subsequent stages of tooth dislocation should be carried out with smooth back-and-forth movements with a gradual increase in the applied force, mainly in the direction in which the tooth being moved encounters less resistance. It is advisable to plan a tooth extraction operation taking into account X-ray data. If, based on the analysis of radiographs, it is determined that the tooth being removed has diverging curved roots, then to prevent a root fracture, it is better to start the operation by crossing the interroot adhesions with a fissure bur, and then sequentially remove each part of the tooth using an elevator or forceps.
Treatment of tooth root fracture
If a root fracture occurs, you should proceed to an atypical tooth extraction operation: • detachment of the mucoperiosteal flap; • access to the root through a burr hole in the area of the vestibular wall of the alveolar process (alveolar part of the lower jaw); • dislocation of the root with an elevator and pushing through the alveolus; • filling the alveoli with an osteotropic drug; • fixation of the mucoperiosteal flap and bringing together the edges of the gums above the alveolus of the extracted tooth with sutures.
Fracture, dislocation of an adjacent tooth
Fracture or dislocation of an adjacent tooth during an extraction operation most often occurs when using forceps with wide cheeks or when removing teeth with an elevator, when the adjacent tooth serves as a support for the instrument. This complication is considered a medical error.
Prevention of fracture or dislocation of an adjacent tooth
Prevention of dislocation of an adjacent tooth is the careful removal of the causative tooth without relying on the adjacent tooth, or when a tooth is dislocated with an elevator, the fulcrum for the instrument should be the edge of the interdental septum, the neck of the tooth, and not the crown. When using a direct elevator, the first stage of tooth dislocation should be carried out mainly by reciprocating rotational movements of the instrument as its blade is inserted between the surface of the tooth and the wall of the alveolus.
Treatment of a dislocated adjacent tooth
If the adjacent tooth is completely dislocated, if it is intact, replantation is possible. If a single-rooted tooth is dislocated, it should be immobilized using a dental wire splint. It is not necessary to immobilize a multi-rooted tooth after replantation. The patient should adhere to a gentle diet and carefully observe the rules of oral hygiene. If tooth extraction was performed due to an acute or chronic infectious-inflammatory process, a course of antibacterial therapy should be administered. The patient should be under dispensary observation with monitoring of the condition of the dental pulp (electroodontometry in dynamics) and the condition of the periodontium (x-ray monitoring after 2, 6 and 12 months). If a fracture of an adjacent tooth occurs, we choose treatment tactics based on the clinical situation: we determine the condition of the hard tissues of the tooth, pulp and periodontium. Assessing the condition of the dental tissues can also help determine whether there were any factors that caused the fracture: periodontal disease, caries, poor-quality fillings.
Tooth crown fracture
A tooth crown fracture is often a complication. It occurs due to the destruction of the crown by a pathological process or due to anatomical features. Increases the risk of traumatic removal of the root remaining in the hole. A fracture of the tooth crown can occur due to incorrectly selected instrumentation and violation of the extraction technique.
Prevention of tooth crown fracture
Prevention of tooth crown fractures lies in the correct tooth extraction technique and strict adherence to the principle of anatomical correspondence of the forceps to the tooth being removed. When fixing the forceps, you should not use excessive force, and tooth dislocation should be carried out with smooth back-and-forth movements with a gradual increase in the amplitude of tooth movement and the applied force. Before removing a tooth affected by caries, a fibrotomy should be performed along the entire perimeter of the root part of the tooth to the maximum possible depth in order to reduce the force required to dislocate the tooth.