Impacted and dystopic wisdom teeth
Teeth characterized by the most delayed eruption are known for a host of problems that they can cause to their owner. The fact is that not every wisdom tooth grows evenly and eventually erupts completely.
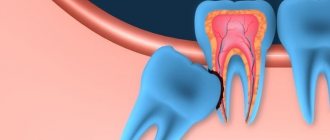
If a tooth is positioned incorrectly, it is called dystopic. We are talking about turning the other side or sprouting at the wrong angle. This phenomenon is observed not only in the growth of wisdom teeth, but also in the rest of the dentition, and therefore can cause significant deviations in bite and significantly spoil the aesthetics of a smile.
Impacted teeth are teeth that are delayed in eruption. Retention is divided by experts into two types:
- Complete, if only bone tissue or the gum itself is visible from the outside.
- Partial, if only part of the tooth is visible, which means that its eruption is not complete.
Very often, dentists can observe not only these defects separately, but both simultaneously. But most often this concerns the third molars. But this also happens with wisdom teeth, although it is considered a very rare occurrence in medicine. Often it can provoke the occurrence of such troubles as periodontitis, periodontal disease, inflammation of the oral cavity and caries.
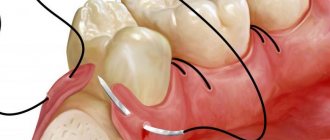
Impacted wisdom teeth can cause pericoronitis, which is characterized by inflammation of the dental crown, accompanied by difficulty and pain when opening the mouth. With this disease, ear pain and even sore throat from the affected tooth may occur. In some cases, the patient suffers from pain in several teeth at the same time, as well as general weakness and fever.
Important! In these cases, the patient necessarily requires a professional examination by a dental surgeon who can excise the inflamed tissue, after which the patient is given appropriate recommendations for wound care.
Indications for extraction of jaw units overgrown with gums
Removal of an impacted tooth is carried out when its abnormal position leads to negative consequences:
- Retention of one tooth impedes the normal growth of the remaining units in the row and leads to malocclusion.
- An impacted tooth injures the cheeks and tongue, which leads to a persistent inflammatory process and ulceration of the oral mucosa.
- Before installing a brace system, when it is necessary to eliminate all the causes leading to a pathological bite.
- For pericoronitis - inflammation in the gum area. A condition when the mucous membrane partially covers the tooth, and infection accumulates under this “hood”, which leads to constant pain and swelling.
- Before installing dentures, when an impacted unit interferes with access to an adjacent tooth.
Important! Before removing an impacted tooth, a person is examined by an orthodontist. If orthodontic treatment is not possible, extraction of the unerupted area is prescribed if indicated.
Removing an impacted tooth means removing it completely from the gum or jaw bone. This procedure is a full-fledged operation, which is often performed in a hospital.
Features of wisdom teeth removal under the gum
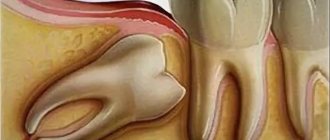
- When planning the course of the operation, it is necessary to determine which teeth lie on the way to the impacted one, since the possibility of their resection or removal cannot be excluded.
- Access to the lower impacted wisdom teeth (eights) is usually made through the vestibule of the mouth.
- When choosing the shape of the incision, preference is given to a semilunar or trapezoidal dissection.
- If there are no adjacent teeth next to the impacted tooth, the incision is made down from the edge of the alveolar process.
- The size of the soft tissue wound should allow free trephination of the bone along the entire length of the impacted tooth.
- Wisdom teeth are removed with special bayonet-shaped forceps, which are more convenient for gripping, since access to figure eights can be difficult due to their location in the oral cavity, and also because they are completely destroyed by caries.
- When dislocating impacted teeth with elevators, the strength of the support should be taken into account and the procedure should be started no earlier than half of the surface is exposed.
- If retention is complicated by osteomyelitis or suppuration affecting the maxillary sinus, additional sinus surgery is performed.
- If the tooth is severely crooked, it is removed in parts.
Why does retention occur?
There are several reasons for this phenomenon:
- Lack of free space due to incorrect alignment of adjacent teeth.
- Supernumerary of the jaw.
- Inflammation or premature removal of baby teeth.
- Improper functioning of the glands that are responsible for internal secretion.
- Incorrect placement of the permanent tooth germ.
- Genetic predisposition, when disturbances in the formation of molars are transmitted hereditarily.
- The absence of neighboring teeth, which determine the correct shape of the dentition.
Features of medical care
If an impacted tooth causes the problems described above, then in most cases it is removed. Removing such teeth is very problematic due to the fact that sometimes the doctor has to cut into the gums in order to gain full access to them. Fortunately, modern dentistry has all types of pain relief, which allows you to minimize discomfort for the patient.
The operation takes place in several stages:
- To remove a tooth, the doctor makes an incision in the mucous membrane.
- A hole of the required diameter is drilled into the bone.
- If the tooth is too large, it should be crushed before removal, since it will be easier to pull out parts than the entire tooth.
- After extracting parts of the tooth, medications are placed into the formed cavity, and if the incision was too large, the gum is sutured.
Important! Experts advise not to delay the removal of impacted wisdom teeth, since various complications in the form of tumors and inflammatory processes are possible. If your wisdom tooth erupts with severe pain, then this is the first sign that you need to see a specialist.
How is an impacted tooth removed?
Removing an impacted tooth is a complex surgical procedure that can only be successfully performed by an experienced dental surgeon. Removing impacted dystopic wisdom teeth is considered especially difficult due to its incorrect position. On average, the procedure itself takes about half an hour, but in particularly difficult situations, tooth extraction can last more than two hours. In addition, it is believed that removing an impacted wisdom tooth in the lower jaw is more difficult than removing an impacted wisdom tooth in the upper jaw. This is explained by the fact that the bone tissue in the lower jaw is denser, so the tooth can be extracted more easily. However, the upper impacted wisdom tooth is removed using the same technology, so there are no big differences here.
Stages of removing an impacted tooth:
- Consultation, diagnostic procedures. Sanitation of the oral cavity. Often, several days before the procedure, sedatives and vitamins are prescribed.
- Anesthesia (general anesthesia, sedation, local anesthesia - depending on the complexity of the case and the wishes of the patient).
- An incision is made and the gum is pulled back to access the bone tissue. Can be performed using a scalpel or laser. The second method is more modern and less invasive, but the cost of the procedure increases significantly.
- Preparation of bone tissue using a special bur to access an impacted tooth.
- Extracting the tooth using special forceps (elevators) or sawing it into several parts and removing each piece separately. The second method is considered more predictable and safe.
- Plastic surgery of soft or hard tissues, suturing (if necessary), treating the area with antiseptic and anti-inflammatory solutions.
Treatment of dystopic teeth
Such anomalies can be treated with orthodontic methods. For example, if you put on braces in time, your wisdom tooth can be returned to its normal position. This process is very long, but the prognosis in most cases is favorable. If the tooth is dystopic due to lack of space in the jaw, then it is recommended to remove it.
What could be the consequences?
If treatment is not carried out on time, the patient may experience the following problems:
- Malocclusion.
- Due to improper positioning of teeth, soft tissue injuries are possible, leading to the development of suppuration.
- Minor diction problems are possible.
What can a dentist offer you?
Most often, the patient goes to the dentist too late. In this case, the dystopic tooth or several adjacent to it are removed. As a rule, correcting such a defect, especially an advanced one, is very difficult, because its location in the oral cavity is somewhat atypical. To make the dentist’s work and your own fate easier, you should not delay your visit to a specialist.
It is very problematic to remove a dystopic wisdom tooth, therefore, to eliminate the defect, the tactic of removing ordinary teeth from a row is used. For example, if you go to the dentist before the age of 15, the solution to the problem will be the mildest: the least important tooth in the row will be removed.
Dear patient!
Thank you so much for your trust, patience and correct attitude towards your health. You have just undergone surgery, tooth extraction, which, by the way, is the most common and frequent surgical procedure in the world. In order to make the subsequent rehabilitation period as comfortable and safe as possible, I ask you to read this leaflet and follow the recommendations and instructions indicated in it.
So,
Usually, after removal, a gauze pad remains in the mouth. It must be removed 30 minutes after surgery.
Why?
Contrary to popular belief, a gauze pad is not used to absorb blood, but to apply pressure to the edges of a wound and stop the bleeding, just as we apply pressure to the edges of a wound on the skin to prevent it from bleeding. Therefore, there is no point in changing the tampon every five minutes “because it is completely saturated with blood.” Moreover, I recommend soaking the tampon in saline solution in advance - this way it will not absorb plasma from the blood clot, and it will form faster and hold better.
By the way, I wrote about this back in 2012. Here >>
What if…
... the bleeding doesn't stop? It's no use changing tampons, it won't get better. It would be more correct to press it harder against the hole (if necessary, add another one) and leave it like that for 30-40 minutes. Repeat if necessary. If the bleeding does not stop even in this case, you need, first of all, to measure your blood pressure (if it has increased, take appropriate medications), and secondly, urgently contact your doctor.
Ice is usually offered as a cold compress after surgery. It is advisable to apply cold compresses every 2 hours for 20 minutes during the first 24 hours after surgery.
Why?
The body responds to any surgical intervention as if it were an injury (yes, for it it is an injury) with an appropriate reaction: bleeding, plethora, release of plasma into the intercellular space of tissues, etc. The vessels in the area of the operation dilate, blood circulation increases - this is why bleeding increases, swelling increases, and the cheek in the area of the extracted tooth becomes hot. Thus, the mechanisms of post-traumatic inflammation are triggered, which, in essence, is the body’s protective reaction to excessive external influence. It is impossible to completely defeat him. And, in fact, there is no need to do this - it’s a defensive reaction! Our task is to keep the postoperative inflammatory process within certain limits, preventing it from developing into something more serious. And here General Frost helps us. Cold compresses prevent swelling from growing, help stop bleeding, relieve pain, and prevent the formation of hematomas. Remember how we apply ice to a bruise or sprain? Here, in essence, we are doing the same thing.
By the way, this is a diagram of the development of the postoperative inflammatory process. This is described in detail here>>
What if…
…. don't apply ice? In fact, nothing bad will happen. It’s just that the swelling and subsequent hematoma will be larger, the blood will stop longer, and the pain will be more intense. Otherwise, the entire postoperative period will follow the same pattern as with ice.
For 2-3 hours after removal, do not eat food or hot drinks.
Why?
Anesthesia! Chewing involves not only teeth, but also cheeks, lips, and tongue. After anesthesia, they all remain insensitive for some time (from half an hour to several hours), which means that when chewing something, we can literally “chew”, burn and seriously injure them. This is especially true for children, to whom it is difficult to explain that they should not bite their lip, even if it does not hurt. But this is just one reason why it is recommended to eat only after the anesthesia wears off.
Do not forget that a wound remains in the oral cavity after tooth extraction. She's bleeding. While chewing even cold food, the temperature in the oral cavity rises and blood flow increases, which will ultimately lead to increased alveolar bleeding and increased swelling in the area of the extracted tooth. In addition, food debris can push through the still soft blood clot and socket, infecting them with all the consequences.
What if…
... do you want to drink and eat after removal? Well, you can drink, for example, cold still water or iced tea immediately after the operation, nothing bad will happen. As for food... it's better not to. Instead of the desired hamburger, drink more water and you’ll see that your hunger will go away. At the same time, you will lose weight).
For 3-4 days, exclude rough, hot, hard, spicy foods.
Why?
As I already wrote in paragraph 2 (about the cold), from the point of view of the body, it does not matter whether the tooth was knocked out in a fight or carefully removed in the clinic - it reacts to the operation as if it were an injury and responds to it with a corresponding protective reaction - inflammation. It is characterized by a number of symptoms of varying severity (see below), which are the source of discomfort in the postoperative period.
Rough and hard food can squeeze a blood clot out of the hole of an extracted tooth, simply push into the hole or injure the mucous membrane around it - and this will in no way contribute to smooth healing. On the contrary, an empty (or “dry”) socket, and even with “food reserves” in it, easily becomes infected - this is how alveolitis occurs, an extremely unpleasant and difficult to treat disease.
Hot and spicy foods increase blood flow in the oral cavity, including in the area of surgery. This, in turn, leads to the formation of edema, hematomas, bleeding, and, even worse, can contribute to the spread of infection, toxins and tissue breakdown products (and there is always one) beyond the area of the operation.
What if…
... really want to eat? For the first few days, it is better to switch to soft, warm foods that do not irritate the oral cavity. These can be various fruit and vegetable purees, porridges, broths, homogeneous soups, steamed fish, steamed cutlets, meatballs, yoghurts, dairy products, soft cheeses, etc. Under no circumstances should you go hungry, since the body needs food from somewhere. take strength to recover. In addition, fasting is additional stress, which does not make the postoperative period any easier.
For several days, it is recommended to limit excessive physical activity, sports, and cancel solarium, sauna, steam bath, and hot bath.
Why?
For the same reason. Exercising, dragging bricks and hilling potatoes at speed creates a load on the cardiovascular system: the heart rate increases (to varying degrees for everyone), blood pressure and body temperature rise. Accordingly, local blood flow in the surgical area increases. And along with it - swelling, the likelihood of bleeding and “pushing” a blood clot out of the hole. The last one is preved, alveolitis! I have already mentioned what alveolitis is. This is extremely unpleasant crap.
Sauna, solarium, hot bath - the same reason.
What if…
... I'm an athlete, and I can't go without training? I also work as a bathhouse attendant in a women’s bathhouse, so I can’t live without a sauna? I assume that over the years of training spent in the sauna, the body has adapted to physical activity and high temperature, so maintaining a normal lifestyle is quite acceptable. But we are talking about excessive physical exertion, which means that for several days after the operation it is better to refrain from setting Olympic records for running in a hot bath. If you run 5 km daily before breakfast, 3-4 days after surgery, slightly reduce the pace and intensity, reducing the distance to 3 km. Your body will appreciate it.
You cannot rinse the area of the extracted tooth, try to rinse it, clean it, etc. You cannot unravel the stitches, try not to disturb the area of the extracted tooth. Stop using the irrigator for a few days.
Why?
Because gladiolus is an alveolite. Let me remind you that after removal, the tooth socket is filled with blood, forming a blood clot - a kind of protective bandage that protects the wound surface from exposure to the external environment, including infection. Subsequently, this same clot grows into vessels and serves as a kind of matrix for the growth of bone tissue. Its safety is not only the key to a comfortable postoperative period, but also to normal conditions for further implantological treatment. Rinsing, especially intense, with the help of which some patients try to get rid of odor or other unpleasant sensations, can lead to the separation and washing out of a blood clot, as a result of which the wound surface remains open, easily becomes infected and inflamed - this is where alveolitis begins, very unpleasant and difficult treatable disease.
What if…
... is there a smell (or something else), does it seem like food has gotten into the hole, etc.? The most correct decision in this case would be to contact your doctor or, at a minimum, have a telephone consultation with him. Trying to get something out of the hole with a toothpick or washing the hole with an irrigator can seriously complicate the postoperative period, since the hole left without a blood clot quickly becomes infected and inflamed. So much for alveolitis.
After removing impacted teeth, supernumerary teeth, and wisdom teeth, sutures are usually placed on the socket. This is usually done using resorbable suture material, so there is no need to remove sutures.
Why?
It’s trivial - to reduce the size of a postoperative wound, fix its edges, seal it from infection from the outside, and keep a blood clot in the wound. To close the tooth sockets after extraction, I use modern resorbable suture material (Vicryl, PGA, etc.). This means that the sutures do not need to be removed; they will be resorbed on their own within 3-4 weeks.
What if…
... the sutures are not resorbed within the specified period? If they don't bother you at all, you can just wait a little longer - they will fall off on their own. If they bother you, irritate the mucous membrane, or it seems to you that they are interfering with the normal healing of the wound, you can come to my clinic in the second or third week after the operation, I will remove them. It's free.
Do not self-medicate, use traditional medicine, or take homeopathic medicines.
Why?
The effectiveness of homeopathic medicines and folk remedies for all diseases is a controversial issue. Let's not argue about this. Moreover, the recommendation why this should not be done lies in the legal and ethical planes.
Your work with the doctor is not limited only to the surgical intervention itself; he is also responsible for your rehabilitation period. Your attending physician, taking into account the nature of the surgical operation and the characteristics of your body, makes prescriptions and gives recommendations that best suit your clinical case. At the same time, the doctor rightly believes that you will comply with them, and this gives him the opportunity to predict the course of the postoperative period and, in case of any problems, make the necessary adjustments. A patient who treats himself is like a driver who bought his license for a bottle of vodka and is not familiar with traffic rules at all - he becomes unpredictable on the road, and it is at least difficult for other people to be responsible for his safety.
What if…
... the doctor does not give any recommendations and runs away immediately after the operation without explaining anything? Try not to let the doctor run away without recommendations and prescriptions. If he still runs away and ignores you in every possible way, you can contact the head of the department or the chief physician. According to the agreement that you signed before starting treatment, you are obliged to comply with the doctor’s recommendations and prescriptions, but if you have not received them, what kind of agreement can we talk about? However, I strongly recommend not to treat yourself, not to receive treatment over the Internet and not to listen to the advice of friends and relatives (at least, coordinate them with your doctor), since the doctor will have a reason to refuse to comply with his obligations under the contract for the provision of medical services. And as a result, he may not be responsible for your treatment.
You need to take the following medications:
– antibacterial therapy. There are more than 100,500 types of various antibacterial drugs; in each clinical case, the doctor selects them individually, based on the indications and state of your health. Typically, antibacterial therapy accompanies the removal of lower wisdom teeth, any impacted teeth, as well as in cases of traumatic or difficult removal, or in cases of exacerbation of the inflammatory process (acute pain, swelling, etc.). I specifically do not write the names of medications here, so as not to provoke attempts at self-medication - I would like to emphasize once again that only your attending physician has the right to prescribe medications for you.
– anti-inflammatory therapy. Usually consists of one or two components: nonsteroidal anti-inflammatory drugs (NSAIDs) and antihistamines (AGS). We often call NSAIDs “painkillers,” rightly believing that their main purpose is to relieve pain. But no. Anti-inflammatory drugs help control the inflammatory process that always develops after surgery, and pain relief is just one of their effects. You need to be extremely careful with anti-inflammatory drugs, do not abuse them, do not prescribe them yourself, because the consequences can be worse. Antihistamines are part of anti-inflammatory therapy, and not a treatment for allergies, as some people think. We prescribe them because the development of inflammation involves factors similar to those that provoke allergic attacks - AGS is needed to relieve them.
– additional drug therapy. Serves both to eliminate the side effects of antibiotics and anti-inflammatory drugs, and to treat the underlying disease. For example, the prescription of NSAIDs to patients with gastritis or gastrointestinal ulcers is often accompanied by antacid medications, and in cases of tooth extraction in the upper jaw complicated by perforation, vasoconstrictor and antibacterial drops for the nasal cavity are prescribed.
– vitamin therapy. For several years I have been practicing the prescription of vitamins to accelerate the regeneration of bone wounds in order to prepare for implant treatment. Again, even such trifles as prescribing vitamins should be taken seriously, since in some diseases and conditions they can cause serious harm.
Again,
Only your doctor can prescribe medications. I strongly do not recommend taking medications without a doctor's prescription.
What if…
... not taking medications at all? Such actions fall under paragraph 7 of these recommendations; this is a direct violation of the contract for the provision of medical services on your part - the doctor and the clinic have the right to decline responsibility for the result of your treatment. And, if any problems suddenly arise, then only you will be to blame.
You need to come for a postoperative examination, usually scheduled for 2-3 days after surgery.
Why?
The most difficult thing in a surgeon’s work is not performing a surgical operation, since even a monkey can be taught to swing a scalpel. In my opinion, the most difficult thing is to ensure that the patient recovers as quickly as possible after surgery, with minimal discomfort and the risk of complications. At the same time, even in one person, the nature of the postoperative period can differ significantly, depending on the characteristics of the surgical intervention, and it is quite difficult to predict how pronounced swelling, hematomas, and pain will be after the operation. A postoperative examination, which is carried out “at the peak of symptoms,” allows you to assess the consequences of the operation and, if necessary, adjust recommendations and prescriptions, therefore, alleviate the patient’s condition.
What if…
... the doctor does not invite you for a post-operative examination, or you are not able to come 2 days after the operation? You should, at a minimum, ask the doctor to leave a phone number and ask where to call and what to do if you have questions or problems. But it’s better, after all, to insist on a postoperative examination - the doctor has no right to refuse you.
Typically, the rehabilitation period after dental surgery takes from 2 to 10 days and may be accompanied by the following symptoms:
– painful sensations may appear immediately after surgery, their peak occurs 6-12 hours after surgery, then their intensity decreases.
– edema, swelling of the operation area usually appears on the second day after surgery, reaches its peak after 48-72 hours, and then decreases.
– pain when swallowing is associated with the development of regional lymphadenitis, may appear immediately after surgery and disappear within 72 hours.
– difficulty opening the mouth is associated with swelling of the intermuscular tissue and irritation of the muscle capsule. It goes away within a few days.
– discomfort when chewing, talking – appears for the same reason as difficulty opening the mouth.
– bleeding from the socket of an extracted tooth can be of varying intensity and continue throughout the day.
– the appearance of a hematoma, “bruise” on the skin in the area of the operation occurs because blood infiltrates the soft tissues around the tooth socket.
– increased body temperature, a natural reaction to the postoperative inflammatory process
– nosebleeds are extremely rare when teeth in the upper jaw, especially eights, are removed.
– deterioration in general health can be either a consequence of the operation itself or a side effect of prescribed medications.
– divergence of the seams on the socket of an extracted tooth sometimes occurs due to stretching of the soft tissues by edema.
These phenomena resolve on their own within 4-10 days, provided that all recommendations and doctor’s prescriptions are followed. If symptoms appear beyond those listed above, you must urgently consult with your doctor and, if necessary, adjust the postoperative rehabilitation program.
Well, the most important rule of any rehabilitation period is that any problem, question or concern is a reason to contact your treating doctor. Remember: as long as you are under the supervision of a doctor and in contact with him, you are safe.
What to do with a problem tooth
The difficulty and danger of removing a dystopic, impacted tooth lies in the fact that it is located inside the gum. Such formation is dangerous for the patient because the tooth may be subject to destruction that will be impossible to cope with.
But despite the complexity of the procedure, it is completely safe and painless for the patient. Modern dentistry is able to provide reliable anesthesia and quick results through the use of professional equipment.