Dental diagnostic methods
The main types of diagnostics include those methods that are mandatory for every patient at a dentist’s appointment. These include taking an anamnesis, visual examination of the oral cavity, percussion (tapping) is often used to determine the soreness of a unit of the dentition, as well as probing, which, using a special instrument (probe), allows you to detect carious cavities, gum pockets or bleeding gums.
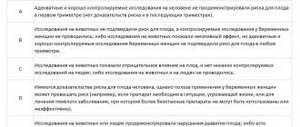
But these methods do not always identify the problem. In this case, additional diagnostic methods are used, such as targeted and panoramic images, computed tomography. Each of these technologies is highly effective in its field and makes it possible to detect the presence of diseases in a short time. Let's consider each of the methods separately.
Risks and benefits of probing around teeth and dental implants
Periodontal probing of teeth is a well-tested method for assessing the patient’s periodontal status, which allows not only to identify areas of inflammation, but also to assess the quality of previous treatment. In addition, using a probe, you can check the condition of teeth in the areas in which periodontal lesions were previously observed, and around which there is an increased risk of developing such pathologies. A periodontal probe can also be used to assess the level of soft tissue recession, verify furcation involvement, assess the mucogingival relationship and diagnose bleeding during manipulation. Since the introduction of prosthetic restorations supported by dental implants, a similar probing approach has been used to check the condition of the surrounding tissue around intraosseous supports. However, given the differences in the anatomy of peri-implant and periodontal tissues, questions remain regarding the safety of probing procedures around titanium screws.
The purpose of this article is to discuss the risks and benefits of probing around natural teeth and dental implants, as well as the advisability of using this manipulation for a more accurate diagnosis of peri-implantitis pathology.
Rationale for probing around natural teeth
Periodontal probing is used to record the depth of existing periodontal pockets and assess periodontal attachment loss. An increase in probing depth over time may indicate the need for additional diagnostic studies such as radiography or checking the level of the bone crest. It must be remembered that there are two parameters of probing depth: biological / histological depth and clinical depth. Biological depth is the distance between the gingival margin and the base of the periodontal pocket, which can only be measured by examining histological sections. Clinical probing depth is the distance to which the probe can penetrate the gingival sulcus or periodontal pocket. Clinical probing depth (CPD) does not correspond to the histological indicator, which differs by an average of 0.3-0.5 mm. However, clinical probing is a non-invasive approach that can provide essential information about the level of periodontal attachment loss and the presence of inflammation in the tissues surrounding the tooth.
CGZ is measured to the millimeter using a graduated periodontal probe with a standard working tip diameter of approximately 0.4 mm to 0.5 mm. The measurement parameters are influenced by such parameters as: the thickness of the probe used; angular positioning of the instrument depending on the anatomical features (photos 1 – 3), probe calibration scale, pressure applied to the instrument during probing; the degree of inflammatory cell infiltration of soft tissues and the concomitant loss of collagen component.
Photo 1. Inadequate position of the probe provokes the acquisition of data regarding the probing depth of 3 mm.
Photo 2: Distal bone loss and tartar.
Photo 3. The correct position of the probe made it possible to diagnose a probing depth of 6 mm.
A decrease in CGZ indicators indicates an improvement in the condition of periodontal tissues. However, only a change in the CGZ indicators after appropriate periodontal therapy does not in itself indicate the formation of a new connective tissue ligament, but rather indicates the completion of the inflammatory process in this area, which, however, can recur without restoration of the histological attachment. A more accurate assessment of the periodontal condition includes, in addition to CGZ, an additional assessment of marginal gingival recession. Subtracting the latter from the former provides a measure of the level of clinical tissue attachment, which can be used to judge the actual loss of periodontal bond. For such measurements, it is necessary to use a certain fixed reference point, which is often oriented towards the area of the cemento-enamel junction. In this way, it is possible to achieve standardization of measurements. Comparison of KGZ data with radiographically recorded loss of the bone crest level is an objective criterion for the loss of hard and soft tissues surrounding the tooth. This information helps determine the prognosis of the affected tooth, as well as the prospective success or failure of its treatment. Bleeding on probing (BP) is another indicator that can be determined using a periodontal probe. A positive PCR result directly indicates gum inflammation. To assess this parameter, index criteria are also available, allowing for a quantitative interpretation of the indicator. CVD alone is not a sufficient predictor of periodontal attachment loss, whereas the absence of bleeding indicates a relatively stable periodontal condition. Changes in probing depth over time and CVD are sufficient to monitor the condition of periodontal tissues both during periodontal lesions and during remission.
Difference between periodontal and peri-implant tissues
The structure of peri-implant soft tissues differs from that of the periodontium around natural teeth. The mucous membrane of the gums around the teeth is covered with keratinized epithelium of the oral cavity, which continuously passes into the connective epithelium. The junctional epithelium ends at the cemento-enamel junction, where acellular extrinsic fibers form the attachment. In this case, collagen fibers pass from the cementum of the tooth into the connective tissue and bone wall of the socket. These structures include gingival, transseptal and periodontal fibers, which provide soft tissue connection to the tooth structure. The soft tissue around the implants consists of a mucous membrane covered with keratinized epithelium, which also continuously passes into the connective epithelium. Apical to the junctional epithelium is a zone of non-infiltrated, cell-free, collagen-rich connective tissue that essentially separates the junctional epithelium from the alveolar bone. This zone, together with the connective epithelium, forms an implant-mucosal junction 3-4 mm long. The connection of the connective epithelium with the surface of the implant is ensured by hemodesmos and the basal lamina. Unlike transcrestal fibers around natural teeth, fibers around implants run parallel to the surface of the intraosseous screw.
Problems associated with probing around dental implants
CGZ and CVD measurements are clinical parameters that are often used to assess dental health (Figures 4 and 5). Given the difference in the anatomy of the peri-implant and periodontal areas, there are certain risks when performing a probing procedure around dental implants. These risks are associated with potential damage to peri-implant tissues, the risk of damage to the implant surface with a metal probe, and the risk of bacterial contamination of the peri-implant area. A discussion of each of these risks is provided in the following sections of the article.
Photo 4. An increase in the depth of probing along with bleeding around the implant indicates the presence of pathology in the peri-implant area and argues for the need to obtain an x-ray.
Photo 5. X-ray data indicate the presence of peri-implantitis.
Risk of damage to peri-implant tissues
The main difference in the structure of peri-implant and periodontal tissues is the absence of fibrous attachment of the peri-implant mucosa to the implant surface. The peri-implant mucosa does not have the same ability to regenerate as the mucosa around natural teeth. However, Etter et al found that after a standardized probing procedure with a force of 0.25 N on the instrument, complete tissue healing was observed 5 days after the manipulation. Thus, the scientists came to the conclusion that probing using a conventional periodontal probe at a pressure of 0.25 N does not cause irreversible damage to soft tissues in a stable condition of the peri-implant area. Therefore, probing remains a reliable and fairly accurate diagnostic procedure that can be used to monitor the state of the mucosal level around installed intraosseous supports.
Risk of damage to the implant surface with a metal probe
Probing of the peri-implant area involves inserting a probe between the supraalveolar part of the implant (implant-abutment interface area) and the mucosa that surrounds it. In this case, the sides of the probe can come into contact with the surface of the implant and rub against its metal neck around the apical third of the abutment. Some studies indicate that such grinding of the probe may cause damage to the implant surface. In the future, these areas can accumulate various bacterial and other contaminants, thus causing the failure of the entire implantation procedure. However, Fakhravar and colleagues, examining roughness on the surface of the apical part of the implant-abutment interface, concluded that probing with a metal probe does not provoke the occurrence of clinically critical effects that compromise the outcome of treatment. In contrast, using magnifying techniques, scientists have found that scalers of different designs (metal and plastic) and plastic probes can have a greater negative effect on the condition of the implant surface compared to conventional metal instruments.
Risk of bacterial contamination
It has been suggested that clinical probing may lead to contamination of soft tissues by various bacteria. The latter can negatively affect the condition of both periodontal tissues and tissues of the peri-implant area. In theory, when a probe is introduced into an area already contaminated by bacteria, bacteria can attach to the surface of the probe and thus be transferred from one area to another. This is how the mechanism of pathogen spread is realized. This transmission mechanism has been shown to be possible in cases of Streptococcus mutans. Light and electron microscopy data support the possibility of bacterial transfer through the mechanism described above, and probes with indentations were found to carry more pathogens than probes with a completely smooth surface. Christersson et al confirmed the possibility of migration of Actinobacillus actinomycetemcomitans on the surface of the probe from the diseased periodontal pocket to the area of periodontally stable tissue. However, even with the persistence of pathogens for 2-3 weeks in the area of healthy soft tissue, no further colonization of the studied area was observed. Holt et al showed that the total colony forming unit was higher in deeper periodontal pockets, so they recommended probing uninvolved or less affected areas first before proceeding to the diagnosis of overt inflammatory areas. Despite evidence of bacterial gavage transmission, Greenstein and Lamster argued in their review of the literature that bacterial transfer in this manner does not necessarily result in colonization or infection of the recipient site, but rather depends on a complex interaction between parameters of host susceptibility, the number of virulent pathogens, state of the local environment and coexisting bacteria. Consequently, the theory of the spread of bacteria and subsequent damage to periodontal tissue and the peri-implant area during probing is not sufficiently substantiated and requires more argumentation.
Risk of galvanic corrosion
Most commercially available dental implants are made of pure titanium (CP-Ti) or titanium alloy Ti-6Al-4V.28, which are highly resistant to corrosion in physiological and acidic environments. This stability is ensured by the stability of the titanium oxide layer. When the stable titanium oxide layer is destroyed and cannot be repaired, titanium becomes as corrosive as other metals used in dentistry.
The risk of galvanic corrosion is that the metal probe may cause the oxide layer on the titanium surface to be removed. After this, in the presence of oral fluid, upon contact between the titanium surface and the probe, an electric current may arise, which develops due to the difference in the potentials of different metals. Galvanic current accelerates the corrosion process of titanium and weakens the structure of the implant. To date, there is only one known case of implant fracture due to galvanic current phenomena. In this case, galvanic corrosion was explained by the use of dissimilar metals in the implant and abutment structure. However, careful use of a smooth, round metal probe, according to some studies, does not provoke the development of galvanic corrosion during diagnostic procedures.
Rationale for probing around dental implants
Although the usefulness of probing around dental implants has been questioned, the consensus report of the Sixth European Workshop on Periodontology recommended that peri-implant tissues should be assessed using the following parameters: bleeding on probing, suppuration, probing depth, radiographs, and implant mobility. Three of these five parameters require the use of a periodontal probe. Examination of the depth of the gingival sulcus is an important step in assessing the stability of the intraosseous structure. Measuring probing depth helps monitor tissue integrity in the peri-implant area, and increasing depth usually indicates loss of alveolar bone support. When probing depth increases and bleeding is present, additional diagnostic procedures must be performed taking into account the potential risk of developing peri-implantitis. An increase in probing depth, accompanied by bleeding without concomitant bone loss, makes it possible to diagnose the pathology of perimucositis. If signs of perimucositis are combined with x-ray evidence of bone loss, the doctor may diagnose peri-implantitis. In addition, probing helps assess the degree of pathology on the vestibular and lingual sides of the implant, which remain invisible on dental radiographs (photos 6 - 8).
Figure 6. The periapical radiograph shows bone loss only on the proximal sides of the implant.
Photo 7. Probing helps to register pathological conditions also on the vestibular and lingual sides of the implant.
Figure 8. During flap separation, significant circumferential bone loss was discovered.
Due to the absence of the periodontal ligament and the loss of bone tissue on the buccal and lingual sides of the implant, we can talk about a circular peripheral reduction of the surrounding residual ridge. Given the differences in periodontal and peri-implant anatomy, a probing depth of 4 mm to 5 mm around the implant is not as critical as around natural teeth (Figures 9 and 10).
Photo 9. The presence of deep pockets around implants without bleeding is not a sign of peri-implantitis.
Photo 10. Deep probing can be caused by the specific landing of superstructures.
However, if there is bleeding, the problem becomes more serious. In such cases, it is important to record changes over a period of time, ensuring that relevant indicators are monitored. When assessing the condition of the soft tissues around implants, it is important to remember that their hemidesmosomal attachment to the surface of the titanium support is weaker, so the pressure during probing should not exceed 0.25 N. Excessive force on the probe can lead to penetration of the instrument into the acellular zone, such Thus, probing the condition of soft tissues can develop into probing the condition of bone tissue. In such cases, the accuracy of diagnosing the pathology of peri-implantitis is impaired. The presence of bleeding upon light probing is another useful criterion for diagnosing inflammation of soft tissues in the peri-implant area. In a pilot study, Lang and colleagues demonstrated that stable peri-implant tissues were characterized by the absence of AGE, while increased AGE parameters were observed in areas of perimucositis (67%) and peri-implantitis (91%). The predictive value of PCR was investigated in a prospective clinical study, in which this indicator showed high negative predictive values. In other words, the absence of bleeding can serve as an indicator of the stability of the soft tissues of the peri-implant area.
Summary and recommendations
Thus, the risk of periodontal probing of natural teeth and tissues surrounding dental implants includes only the possibility of contamination of these areas with the further spread of pathogens. Incorrect probing can lead to inadequate diagnosis of pathologies. Due to the less strong connection of the connective tissue attachment in the area of the implants, the doctor may inadvertently provoke probing of the levels of the surrounding bone tissue, instead of the area of the surrounding gums. Carrying out this diagnostic procedure around teeth after surgery before the tissue has healed, or around implants before the osseointegration process is complete, has the potential to disrupt the regeneration process. Today, the installation of implants is becoming an increasingly common surgical procedure. It was found that 45% of patients after implantation show signs of damage to peri-implant tissues of varying severity. The presence of clinical signs of such disorders is critical, and the probing procedure in such cases remains the optimal non-invasive method for screening the condition of peri-implant and periodontal tissues.
To adequately implement this diagnostic method, the following recommendations should be followed:
- use a smooth probe with a round tip with a diameter of 0.4 mm to 0.5 mm;
- during probing, use only light force of no more than 0.25 N;
- After probing clearly affected areas of tissue, the probe should be cleaned in a chlorhexidine solution (for example, in areas of abscesses, peri-implantitis with exudate) before using the instrument to probe other areas in the same patient.
To record the objective state of tissues, it is necessary to adapt the position of the probe based on anatomical conditions. If there are different types of splints or hybrid prosthetic structures, it is difficult to achieve a similar result (photo 11), therefore, if possible, these devices should be removed from the oral cavity for the period of probing. If it is impossible to remove them, it is necessary to photograph the position of the probe and repeat it during the re-inspection. Accurate assessment of soft and hard tissue loss can only be achieved by using a fixed reference point, such as the level of the cemento-enamel junction, the edge of a vacuum formed stent, or the implant-to-abutment transition area. Also, for this purpose, you can use a vacuum-formed stent (photo 12), against which the necessary areas of probing are determined and study parameters are recorded.
Figure 11: Prosthetic design that limits probing options around implants.
Photo 12. Stent to standardize the probing procedure around implants.
conclusions
Periodontal probing remains the most effective and non-invasive method for diagnosing the condition of supporting dental structures. The presence of bleeding upon probing indicates the presence of inflammation. The use of a probe also helps determine the level of marginal recession and evaluate the periodontal treatment performed. When using probing indicators together with an x-ray, it is possible to determine the prognosis of the tooth, as well as diagnose the presence of plaque or calculus. Probing around dental implants is also a non-invasive method for diagnosing abnormalities in the peri-implant area, which helps justify the need for radiography. Together with the assessment of CVD, pus drainage and radiographs, probing can be used to determine the severity of peri-implantitis, to guide the choice of treatment (surgical or non-surgical), and to evaluate the results obtained. Data obtained from probing periodontal tissue and the peri-implant area are an important clinical indicator for assessing the patient’s periodontal status, the degree of pathological disorder and loss of soft tissue attachment.
Authors: Stuart J. Fromum, DDS Wendy CW Wang, BDS, MSc
Photo of a tooth on Molodezhnaya
Research price 350 rubles
This type of diagnosis is performed using a radiovisiograph, which allows you to assess the condition of one or two teeth. In this case, it is possible to determine the presence of caries, monitor work during the treatment process, and assess the condition of the implant being implanted. A targeted dental image has a number of important advantages:
- has high resolution
- low price for this type of diagnostics
- the patient receives a low dose of radiation
However, a significant disadvantage of this method is the limitation of its angles. This may cause some distortion of shapes or sizes in the pictures. For a reliable result, the experience and professionalism of the specialist who conducts it is important, so you should contact trusted clinics with highly qualified doctors.
When should you undergo a general examination by a dentist?
Experienced dentists and orthodontists strongly recommend visiting a dental clinic for a preventive examination at least once every 6 months. This should be done even if there are no complaints. If you have any unpleasant sensations, you should not delay your visit to a medical facility for even a minute.
There are several main causes for concern: increased sensitivity of the enamel, pain in the gums under the denture, swelling, redness and any other visible tissue changes. Also, one of the symptoms of developing pathology is a strong smell from the mouth, which does not disappear even after brushing.
Abundant accumulation of plaque and tartar, changes in the shade and transparency of the enamel, bleeding - all this is a good reason to visit your doctor. Also, consultation and examination are required before orthodontic treatment.
previous post
Why are my teeth numb?
next entry
Orthopantomogram Youth
The price of the study is 1300 rubles
Or in other words, a panoramic shot. Represents an image of both jaws. The image also shows the surrounding soft and bone tissue. All this allows the doctor to fairly fully diagnose dental diseases - determine the presence of caries, damage to the tooth root, identify cysts, impacted teeth and much more. A panoramic image today is considered one of the most common diagnostic measures, since its price is relatively low, and the result allows for a correct diagnosis.
Modern X-ray methods of dental diagnostics show their high efficiency and are absolutely safe for human health.
Percussion (tapping)
Percussion with tweezers or a probe handle along the crown of the tooth allows you to determine the location of the area affected by inflammation. Any examination begins with healthy teeth; for this purpose, the edges responsible for cutting and chewing reflexes are tapped on the top and sides of the crown.
The process of tapping teeth (percussion)
A good idea of where the source of inflammation is located is given by the relationship between the nature of the pain and the direction of the blow: periodontitis is detected with a horizontal blow, damage to the root nerve can be determined with a vertical blow. Thanks to this technique, the doctor has the opportunity to identify the place where there is pain and prescribe the necessary treatment.
CT dental scan Youth
The price of the study is 3900 rubles
Computed tomography allows you to obtain a three-dimensional image of the dentition in just one scan, which makes it possible to make the most accurate diagnosis, select a suitable implant, and also monitor the results of the work performed. The main advantages of the technique are:
- high quality of the resulting images
- short impact – the procedure lasts less than one minute
- low probability of errors during examination
- Possibility of repeating the procedure due to low radiation exposure
Stages of diagnostics
Carrying out a set of diagnostic measures to determine dental diseases has several stages:
- Taking anamnesis and assessing the condition of the oral cavity using examination, percussion and probing;
- Study of the condition of previously placed fillings and prostheses (implants);
- Bite study;
- Performing hardware diagnostics (OPTG, X-ray, CT);
- Making a diagnosis, discussing future treatment options with the patient and drawing up a treatment plan.
Such a complete diagnosis allows you to study in more detail the condition of all the patient’s teeth in order to prescribe competent treatment.